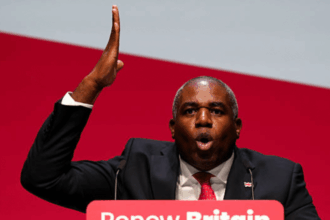
When Tom Hanks appeared on The Late Show with Stephen Colbert on November 3, the host asked why he still wears a mask:
I’m doing a play right now so I cannot get sick… I’ve had COVID enough in my life, I don’t need to do that again. So I’m wearing this for health reasons.
That comment came in the context of his starring and co-writing role in This World of Tomorrow, an Off-Broadway production at The Shed. Hanks had recently been photographed riding the New York City subway while wearing a face mask, first a surgical mask, later a high-filtration KN95.
Stephen Colbert and the ongoing COVID-19 pandemic
Stephen Colbert’s late-night career has also intersected deeply with the ongoing pandemic, recording a monologue from his bathtub when studios first shut in March 2020 and then running extended stretches of the program from outside the Ed Sullivan Theater, including remote a setup at the family home in South Carolina.
By late 2023, The Late Show had weathered multiple COVID-related interruptions, first in April, then in October. A few weeks later, in November 2023, the situation escalated when Colbert underwent emergency surgery for a ruptured appendix, lost 14 pounds, and described how he “was not aware of the amount of trouble I was in.”
When he returned in December 2023, according to his own account, Colbert had taped two episodes while in severe pain, rehearsed his monologue with a “barf bucket” beside his desk, and only later learned that his appendix had burst and caused blood poisoning. Colbert’s health scare, and its proximity to the show‘s COVID cancellations, raises an important question: could his acute appendicitis and subsequent complications relate in part to the infection a few weeks before?
While no individual case allows for definitive causal attribution, a growing body of clinical research suggests that infection with SARS‑CoV‑2 (the virus that causes COVID) is associated with health complications beyond the airways, including increased risk of acute or complicated appendicitis.
Biological association between COVID and organ damage
Early in the pandemic, an increase in acute appendicitis cases was often attributed to delayed care during lockdowns, but newer understandings of COVID’s effects on the body add weight to a direct biological association.
Many people continue to think of COVID‑19 as an upper respiratory infection, like a cold or flu, but it has become increasingly clear that the illness is a multisystem, neurovascular disease. SARS-CoV-2 is not limited to the airways because it targets the endothelium, the thin layer of cells that lines every blood vessel in the body. Reviews in Nature outline how SARS-CoV-2 can damage the lining of blood vessels (the endothelium), set off tiny clots (micro-thrombi), and drive “immunothrombosis,” a feedback loop between inflammation and coagulation that can impair blood flow in multiple organs, including the brain and gut.
A spreading disaster
Once the virus, or the inflammation it triggers, damages that lining, the effect can spread through the entire vascular network, essentially the body’s distribution system for oxygen, nutrients, and immune signals. When those blood vessels become inflamed or clogged with tiny clots, all of the body’s systems can be affected. This is why complications range from neurological symptoms to gastrointestinal inflammation and organ injury.
The gut is an essential part of that overall clinical picture. Direct intestinal involvement, persistent immune activation, and signs of a weakened barrier in the GI tract persist after infection, changes that make local tissues more vulnerable.
Those same mechanisms help explain why there has been an increase in complicated cases of appendicitis since the beginning of the pandemic. Lymphoid tissue in the appendix swells after viral infection (a common trigger for blockage), while vascular and immune effects can speed progression from early irritation to perforation or abscess. All of these point to a biologic pathway of injury (rather than simply delays in care) in patients who go on to present with appendicitis that is unusually severe or complicated.
This overall biological picture of COVID as a multi-system disease with downstream effects on the appendix been borne out in the clinical research.
COVID and complicated appendicitis: did this affect Stephen Colbert?
Across a growing number of studies since the beginning of the pandemic, SARS-CoV-2 infection has been associated with a higher risk that appendicitis will present as, or progress to, a complicated course, even after accounting for delays to presentation or surgery.
A 2025 study found that, the rate of complicated appendicitis rose significantly, even after adjusting for treatment-delay factors. A 2024 multicenter retrospective study of adult patients found that SARS-CoV-2 infection raised the odds of complicated appendicitis by more than 3 times while a nationwide study in Japan describe faster progression and a larger share of perforations and abscesses.
While one cannot definitively say that Stephen Colbert’s hospitalization for acute appendicitis was caused by prior COVID infections, the broader literature suggests the infection may have been an additive risk factor, either by promoting inflammation or weakening immune-tissue resilience. COVID may or may not have directly “caused” the crisis, but it plausibly made it more likely, more severe, and harder to recover from.
Cognitive impacts
While appendicitis illustrates how COVID-19’s systemic effects can manifest suddenly in an acute medical emergency, much of its longer-term impact is less visible, but still serious. Because COVID is a multi-system, neurovascular disease, affecting organs including the blood vessels and the brain, many of its consequences unfold gradually.
Among the most widely documented are the virus’s cognitive effects, sometimes described as “brain fog” or post-COVID cognitive impairment, conditions that can persist for months, years or indefinitely after infection.
Tom Hanks’s on-air admission that he has “had COVID enough in my life” and his remark that, as a co-writer of his play, he “disappeared the other night” by forgetting his own lines, intersects with this emerging evidence of COVID’s cognitive effects. SARS-CoV-2 infection leaves measurable marks on the brain and cognition.
Some areas, especially those involved in memory and decision-making, can become slightly thinner or show signs of disrupted connections after infection. This happens because the virus and the body’s immune response can inflame or damage the tiny blood vessels that feed brain tissue, or, in some cases, may directly affect brain cells themselves.
Loss of grey-matter thickness
The UK Biobank imaging study in Nature detected loss of grey-matter thickness and tissue changes in regions tied to memory and smell among people scanned before and after infection, while matched controls without COVID did not show the same pattern.
Complementing the imaging data, a large observational study in The New England Journal of Medicine reported persistent, objectively measurable deficits in attention, memory, and executive function after COVID-19 that, in some individuals, were comparable to the decline seen over years of aging.
For a nightly performer like Stephen Colbert, whose craft relies on sustained presence, even modest cognitive deficits may translate into changes in delivery.
Indeed, some long-time viewers have anecdotally remarked that Colbert’s pacing and energy feel subtly different since late 2023, though such observations remain speculative and could reflect many variables. What cannot be dismissed is the convergence of a serious health event and a virus known to affect cognition.
Personality changes with neurological causes
The lasting effects of COVID infections may extend beyond memory and cognition into changes in personality, including reduced empathy, increased irritability and diminished self-awareness.
Neuroimaging and neuro-inflammation studies offer potential mechanism. For example, a PET-scan study found increased glial activation (gliosis) in the prefrontal cortex, hippocampus and dorsal striatum of persons with post-COVID depressive/cognitive symptoms, linking persistent immune-mediated inflammation to regional brain injury.
A December 2024 BMC Infectious Diseases survey of 114 long-COVID diagnosed participants found that 94.7% reported cognitive changes and a high proportion reported sleep disturbances, depressive symptoms and perceived personality shifts. Higher “neuroticism” and lower “conscientiousness” scores correlated with worse outcomes.
Together these findings mean that, beyond what people call “brain fog,” the virus may disrupt the very neural circuits that regulate emotion. When those systems are impaired, changes in personality make sense as clinical sequelae of a multi-system disease.
Disease insight: neurological over logical reasoning
One of the stranger and more sobering aspects of the ongoing COVID-19 pandemic is the cultural narrative: even as the scientific evidence of SARS-CoV-2’s continuing dangers has become stronger, public awareness is not keeping pace.
A partial explanation is external. Misinformation and disinformation about the virus’s ongoing risks continues to circulate through platforms and search engines, and long debunked conspiracy theories like “immunity debt” still are widely held. This may explain why Tom Hanks’s saying on national television that he wears a mask because he has “had COVID enough” can feel startling for some.
Yet there may be a more unsettling layer to this public health communication gap.
Disease insight (or anosognosia in the neurological literature) describes a patient’s ability to recognize that they are ill. In many neurological conditions, including certain forms of dementia and brain injury, this capacity is diminished or absent. It isn’t denial in the psychological sense, but a structural change in brain function.
It occurs in some frontotemporal dementias, in stroke survivors, and in people with medication-related brain injury, including from benzodiazepines (e.g. Valium/Diazepan, Klonopin/Clonazepan, Xanax, etc.), drugs that ironically are now often prescribed for common COVID sequelae, including anxiety, insomnia, and inflammation control.
Huge complications
In practice, this means that even when patients are told they have a condition, or even when its symptoms are visible to others, they may not believe it. Even when presented with accurate data or clear medical explanations, their brains may reject that information not logically, but neurologically.
This idea that neurology can override psychology may be uncomfortable—and taking it seriously calls for an expansion of what “misinformation” might mean. It suggests that the struggle to maintain public understanding of COVID’s ongoing impact may not only be about bad faith actors, but also about subtle biological effects that interfere with comprehension itself. This calls for approaches to public health communication that combine rigorous citations with factually-grounded pathos.
The appeal to a core self is a concept that exceeds virology, but Stephen Colbert might recognize as adjacent to metaphysics, maybe what Thomas Aquinas might call “essence“ or fundamental nature. Something that is inviolable, even by a pathogen as comprehensively destructive to the biological self as SARS-CoV-2.
An urgent question for soteriology (the theological inquiry into salvation), as well as neurology, could be posed like this: is there a self who can comprehend the ongoing dangers of the pandemic when the physiological capacity may have vanished?
COVID as accelerant and additive risk
While the question—did COVID almost kill Stephen Colbert in 2023?—cannot be answered definitively, the weight of medical and epidemiological evidence suggests that COVID-19 likely played an indirect but meaningful role in shaping the conditions that made his late-2023 health crisis more dangerous. It was probably not the sole cause, but one probable accelerant.
From the start of the pandemic, public understanding of risk has often stopped at the acute phase of infection and that vaccination has neutralized potential damage. Vaccination remains vital because it sharply reduces the odds of hospitalization and death during the acute phase, but it does not prevent infection or the cumulative multi-system damage that can follow.
This is why an infection can lead to secondary events that appear, on the surface, to be unrelated.
A viral assault
A viral assault on blood vessels and immune system can tip a minor intestinal irritation into a case of appendicitis that progresses faster or heals more slowly. The same systemic injury can also chip away at health more quietly, producing changes that are not immediately life-threatening but still profound, including cognitive decline and, in some cases, measurable changes in personality.
Because COVID affects cognition and insight, a society with widespread infection may also find it harder to recognize or act on that fact. This article has aimed to stay cautious and evidence-based, grounding its claims in rigorous science rather than speculation.
But if we take seriously what those data suggest, that repeated infections can erode our collective ability to remember, empathize, and reason, then responding to COVID’s long shadow requires emotional honesty about what we are losing if we don’t act, and how we might regain some ground of human dignity, even if we’re neurologically compromised.
For that reason, the final “Word” goes to someone who once helped the United States make sense of crisis through embodying our shadow.
The final ‘Word’ from Stephen Colbert
“Stephen Colbert”: Nation, tonight’s Word is—
[On-screen graphic: “COVID”]
They say COVID can cause memory loss. Which is great news for anyone who still remembers the past decade.
[Measured in milligrams of Effexor]
But the brain is a muscle. You rest it, it comes back stronger.
[Definitely not a muscle]
Wait… what was I… ?
[On-screen flickers]
Anyway, some people worry COVID changes your personality. To which I say: nonsense! I’m the same brilliant, humble, God-fearing patriot I’ve always been.
[Foolish consistency]
Sure, sometimes I flub a guest’s credits, or which version of me is hosting tonight… but that’s just because I’m evolving.
[Like a virus]
Science calls it “cognitive decline.” I call it “staying on brand.”
[Truthiness forgets selectively]
See, truth is like the sense of smell. You don’t need it to breathe, but you sure miss it when it’s gone.
[Would I smell the house burning down at 3 a.m.?]
Now, some folks say repeated infections might make us less empathetic, more self-centered. To which I say: Finally, some good news!
[America but EXTRA]
Because empathy is a gateway drug to compromise, and I can’t have that clouding my brand. I built this persona one unexamined certainty at a time.
And no microbe is taking that away from me.
[How would you know if it already had?]
People call that ego. I call it gravity. Stars have it.
[And then they collapse]
But maybe—stay with me—maybe there’s a… thinner place now between the person and the performance.
[Somewhere in the pre-frontal cortex]
Maybe the part that believes I was born to hold the center—
[Congenital megalomania]
—is getting louder to cover for the part that can’t remember why.
[And maybe the tinnitus]
Sometimes I feel… like I’m doing an impression of myself doing an impression of me.
[Wear a face mask or your face as a mask. You choose.]
So promise me something. If, one night, the laugh arrives and I don’t…
Don’t clap.
[Hold]
Call me by my name.
[“Stephen Colbert” or Stephen Colbert?]
And if I don’t answer right away—
[We’ll wait, but the epidemiological clock is ticking]
…keep the cameras rolling. I’ll find my way back.
[Through the fog]
It’s fine. It’s nothing. It’s… what were we—
[COVID]
Right. COVID. The word we keep shrinking to fit into headlines.
[Can the soul shrink…?]
Anyway, the important thing is: I’m fine. I’m fine. We’re ALL FINE. And if we’re not, I hereby declare a new normal.
[Mission Accomplished (…again)]
Because in the end, America, COVID doesn’t change who we are—
it just helps us forget who that was.
[“The Word” logo, static-glitch fade-out]
Featured image via the Canary